Premium Only Content
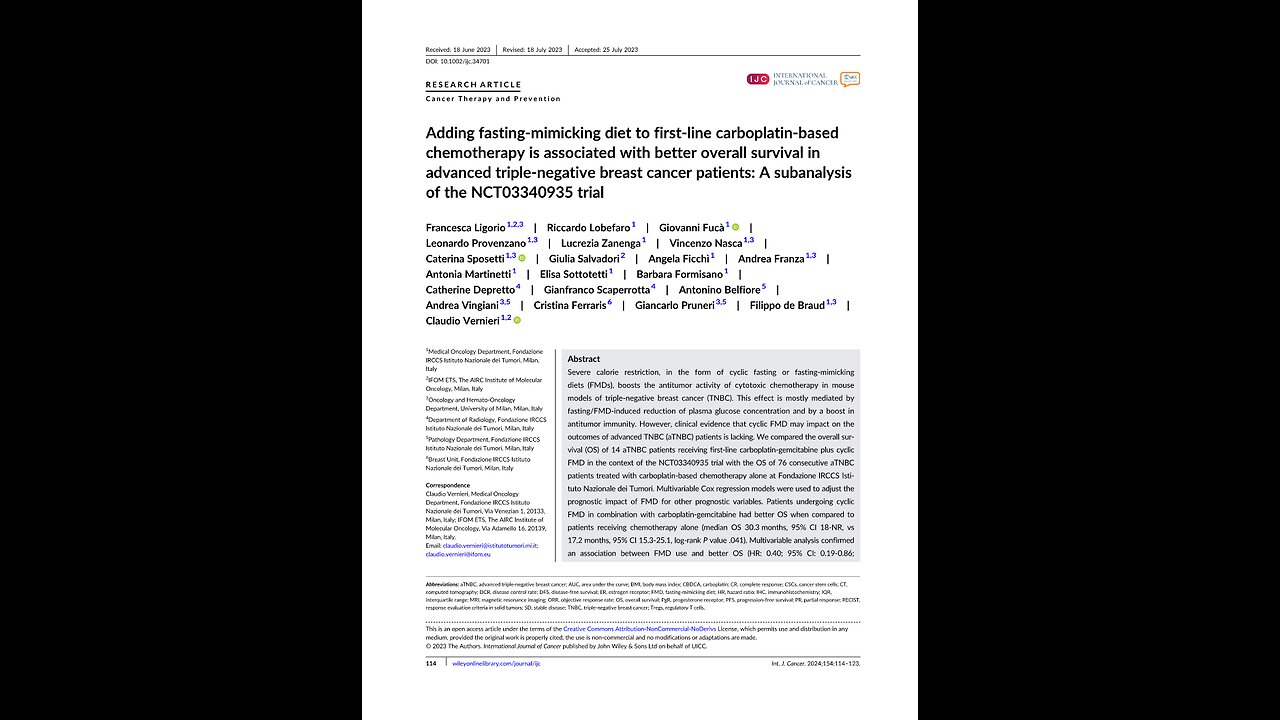
Fasting-mimicking and breast cancer, Claudio Vernieri 2023
Adding fasting-mimicking diet to first-line carboplatin-based chemotherapy is associated with better overall survival in advanced triple-negative breast cancer patients: A sub analysis of the NCT trial.
Claudio Vernieri, and others.
Medical Oncology,
The AIRC Institute of Molecular Oncology,
Milan, Italy.
Abstract.
Severe calorie restriction, in the form of cyclic fasting or fasting-mimicking diets, FMD’s, boosts the antitumor activity of cytotoxic chemotherapy in mouse models of triple-negative breast cancer, TNBC. This effect is mostly mediated by fasting, FMD-induced reduction of plasma glucose concentration and by a boost in antitumor immunity.
However, clinical evidence that cyclic FMD may impact on the outcomes of advanced TNBC, aTNBC, patients is lacking. We compared the overall survival, OS, of 14 aTNBC patients receiving first-line carboplatin-gemcitabine plus cyclic FMD in the context of the NCT03340935 trial with the OS of 76 consecutive aTNBC patients treated with carboplatin-based chemotherapy alone at Fondazione IRCCS Istituto Nazionale dei Tumori. Multivariable Cox regression models were used to adjust the prognostic impact of FMD for other prognostic variables.
Patients undergoing cyclic FMD in combination with carboplatin-gemcitabine had better OS when compared to patients receiving chemotherapy alone, median OS 30.3 months, 95 percent Confidence Interval 18 NR, versus 17.2 months, 95 percent Confidence Interval 15.3 to 25.1, log-rank P value .041.
Multivariable analysis confirmed an association between FMD use and better OS, HR: 0.40; 95 percent Confidence Interval: 0.19 to 0.86.
P equals .019, also after propensity score-based matching according to patient ECOG PS and the presence of de novo metastatic disease. HR: 0.41; 95 percent Confidence Interval: 0.21 to 0.83.
P equals .013.
Cyclic FMD in combination with first-line chemotherapy may improve clinical outcomes in aTNBC patients. Our study paves the way for conducting phase Two trials to investigate if cyclic FMD can increase the antitumor activity, efficacy of chemotherapy or chemo immunotherapy in patients with early-stage TNBC or aTNBC.
KEYWORDS. advanced triple-negative breast cancer, fasting-mimicking diet, objective response rate, overall survival, progression-free survival.
What's new?
Cyclic fasting-mimicking diet enhances chemotherapy antitumor activity in triple-negative breast cancer mouse models. Here, the authors compared the overall survival of 14 advanced triple-negative breast cancer patients receiving chemotherapy plus fasting-mimicking diet within the NCT trial with the overall survival of 76 patients treated with chemotherapy alone. Patients receiving chemotherapy plus fasting-mimicking diet had better overall survival when compared to patients treated with chemotherapy alone. The findings pave the way for future phase Two trials to investigate fasting-mimicking diet activity and, or efficacy in triplenegative breast cancer patients
One. INTRODUCTION.
Advanced triple-negative breast cancer (aTNBC) is a highly aggressive malignancy, and it is characterized by poor patient survival.
Although new therapeutic strategies, such as chemo-immunotherapy combinations in patients with PD-L1-positive disease, trastuzumab deruxtecan in patients with HER2-low tumors or Sacituzumab govitecan, significantly improved clinical outcomes when compared to standard therapies, aTNBC remains a deadly disease for the vast majority of patients, and median OS is lower than 2 years after diagnosis of metastatic disease. Therefore, there is an urgent need to find new and effective therapeutic strategies to treat aTNBC patients.
Preclinical in vitro and in vivo studies published in recent years consistently showed that TNBC cells are exquisitely sensitive to nutrient deprivation. Specifically, combining in vivo nutrient starvation, in the form of cyclic fasting or fasting-mimicking diet, FMD, with cytotoxic chemotherapy, immunotherapy or PI3K AKT mTORC1 inhibitors slowed down in vivo tumor growth and resulted in significant prolongation of animal survival.
In syngeneic mouse models, fasting FMD-induced reshaping of the immune microenvironment, including an increased infiltration by CD8 plus T cells and a reduction of immunosuppressive regulatory T cells, Tregs, was found to crucially mediate the antitumor effects of nutrient starvation, alone or in combination with chemotherapy.
We recently published the results of a prospective, phase Ib trial, which showed that a severely calorie-restricted, 5-day FMD regimen is safe and well tolerated when combined with standard treatments in patients with different tumor types. In addition, the FMD caused a significant decrease in blood glucose, insulin and IGF-1 concentration, thus recapitulating metabolic changes that mediate the antitumor effects of FMD in preclinical models. More importantly, the FMD globally reshaped systemic and intratumor immunity, and in particular, it caused a significant reduction of immunosuppressive populations of myeloid cells and regulatory T cells, which was paralleled by an increase of cytotoxic T lymphocytes, NK cells and memory T cells. Overall, these results confirm and expand results of previous experiments conducted in syngeneic TNBC mouse models. In some patients with highly aggressive and deadly malignancies, we also observed complete and long-lasting tumor remissions, thus suggesting that cyclic FMD could improve the antitumor efficacy of standard therapies in specific clinical contexts.
Among breast cancer subtypes, TNBC is the most immunogenic one, as it is characterized by a relatively high mutational burden and by a highly immune-infiltrated microenvironment. In addition, higher T-cell infiltrate in human TNBCs is associated with higher tumor responses to neoadjuvant chemotherapy. For these reasons, the immunomodulatory effects of cyclic FMD that were reported in TNBC-bearing mice and in cancer patients could have profound therapeutic implications, as also suggested by results of preclinical studies. Recently, FMD-induced reduction of blood glucose concentration was also found to reduce TNBC cancer stem cells, CSC’s, which play a crucial role in mediating tumor resistance to standard therapies. For these reasons, aTNBC patients could especially benefit from a combination of standard chemotherapy or chemo immunotherapy with cyclic FMD.
To test this hypothesis, in the present subanalysis of the NCT trial we selected aTNBC patients treated with first-line carboplatin CBDCA based chemotherapy in combination with cyclic FMD, and we compared their clinical outcomes with survival outcomes in a control cohort of consecutive aTNBC patients treated with standard platinum-based chemotherapy in our institution.
Two. MATERIALS AND METHODS.
Section two point one. Patient population.
The NCT trial was a monocentric, prospective, phase One-b clinical trial that enrolled cancer patients with different tumor types and stages. The study aimed at investigating the safety, feasibility, metabolic and immunomodulatory effects of cyclic FMD in combination with standard antineoplastic treatments, including chemotherapy, radiotherapy, immunotherapy, endocrine treatments, molecular targeted therapies or best supportive care. The FMD regimen evaluated in the NCT trial consisted of a 5-day, calorie-restricted, up to 600 kilo calories on day 1, up to 300 kilo calories on days 2, 3, 4 and 5, low-carbohydrate, low-protein dietary intervention that was repeated every 21 to 28 days, up to a maximum of eight consecutive cycles.
Data about the safety, feasibility, metabolic and immunomodulatory effects of cyclic FMD in patients enrolled in the NCT trial have been recently reported.
For the present analysis, we selected a subcohort of NCT trial patients fulfilling the following criteria:
(One) pathologically confirmed diagnosis of TNBC, as defined as less than 10 percent of cancer cell expressing estrogen receptor (ER) and progesterone receptor (PgR) by immunohistochemistry (IHC) analysis, and either a IHC score for HER2 expression of 0 to 1 plus, or an IHC score of 2 plus in the absence of HER2 gene amplification by in situ hybridization (ISH),
(Two) advanced stage, as defined as metastatic or locally advanced, inoperable disease;
(Three) treatment with CBDCA-based doublet chemotherapy as a first-line treatment for advanced disease. In detail, the two following platinum-based regimens were considered: CBDCA at an area under the curve (AUC) of 2 plus gemcitabine 800 milligram per square meter, both administered I v on days 1 and 8 every 21 days.
CBDCA at an AUC of 5 on day 1 every 21 days plus gemcitabine 800 milligram per square meter on days 1 and 8 every 21 days.
Or CBDCA AUC 2 plus paclitaxel 80 milligram per square meter, both administered I v on days 1 and 8 every 21 days;
(Four) no previous systemic treatments for advanced disease. As a control population, we included a retrospectively collected cohort of consecutive aTNBC patients treated with the same CBDCA-based regimens at Fondazione IRCCS Istituto Nazionale dei Tumori (Milan, Italy) between April 2007 and April 2021.
Section Two point two. Objectives of the study.
The objectives of the present study were to evaluate the antitumor efficacy and activity of cyclic FMD in combination with first-line CBDCA based chemotherapy as a treatment of aTNBC. The primary study end point was Overall Survival, OS, as defined as the time between treatment initiation and patient death from any cause. Progression-free survival, PFS, objective response rate, ORR, and disease control rate, DCR, were secondary study endpoints. PFS was defined as the time between treatment initiation and disease progression, or patient death from any cause, whichever occurred first. ORR was defined as the proportion of patients obtaining partial response (PR) or complete response (CR) as their best response, while DCR was defined as the proportion of patients achieving CR, PR or stable disease (SD) as their best response. Radiological tumor responses were assessed by computed tomography (CT) scans or magnetic resonance imaging (MRI) using response evaluation criteria in solid tumors (RECIST), version 1 point 1.
Section two point three. Statistical analyses.
For descriptive analyses, the median and interquartile range (IQR) were reported for continuous variables, while categorical variables were summarized as percentages. The χ2 and the Fisher exact tests were used to study the distribution of categorical clinical characteristics in patients receiving and not receiving FMD, while the Wilcoxon rank sum test or the t-test were used to compare the distribution of continuous variables in the two patient groups, as appropriate.
Survival curves were represented through the Kaplan-Meier method and compared using the log-rank test. Median survival in months and corresponding 95percent CI’s were provided. Follow-up time was estimated through the reverse Kaplan-Meier method. The association between FMD use, or other established prognostic factors, meaning, age, ECOG PS, body mass index, BMI, previous taxane or anthracycline exposure, presence of de novo advanced disease, number of metastatic sites, presence of lung, liver or brain metastases, and OS or PFS was first assessed through univariate Cox proportional hazard models. Covariates showing a statistically significant association with the risk of patient death or disease progression at univariate analysis were included in multivariable Cox regression models to assess their independent association with OS, PFS. Hazard ratios, HR’s and relative 95 percent CI’s were provided.
ORR and DCR in patients receiving and not receiving FMD were compared to a chi squared test. In all multivariable Cox models, we verified that the assumption of proportional hazards was globally satisfied.
To minimize the potential impact of imbalances between treatment groups, meaning, FMD versus no FMD, on clinical outcomes, we used the propensity score methodology. In particular, we adjusted the association between the treatment received, FMD plus chemotherapy versus chemotherapy alone, and OS or PFS for the likelihood that a patient had of receiving that treatment, given specific baseline characteristics, covariates. As covariates for propensity score matching, we selected:
(a) ECOG PS, as it was the only covariate independently associated with OS in the multivariable model; (b) the diagnosis of de novo metastatic BC, as the only covariate unequally distributed between patients receiving and not receiving FMD.
All statistical tests were two-tailed, and a P-value less than .05 was considered statistically significant. Statistical analyses were performed using R Studio software.
Three. RESULTS.
Section three point one. Patient population.
Among 101 patients enrolled in the NCT trial, 14 patients had aTNBC and were treated with first-line CBDCA-gemcitabine in combination with every 3 week FMD.
The control cohort consisted of 76 consecutive aTNBC patients treated with first-line CBDCA-based chemotherapy doublets between April 2007 and April 2020, Figure 1.
Patient and tumor characteristics are summarized in Table 1.
Median patient age in the whole patient cohort was 55 years (IQR 47 to 67). Patients included in the control cohort received CBDCA plus gemcitabine or CBDCA plus paclitaxel in 25 percent or 75 percent of cases, respectively. Patient receiving FMD were significantly more likely to have been diagnosed with de novo metastatic disease as compared to patients in the control cohort (36 percent versus 5.3 percent, chi-squared test P value equals .004). Other clinical variables were similarly distributed between the two patient groups; importantly, the average number of subsequent lines of systemic treatment was similar in the two groups (mean: 1.64 in the FMD cohort and 1.85 in the control cohort, t-test P equals .70), and no patients received antibody-drug-conjugated ADC based treatment after the detection of tumor progression to the first line treatment.
Patients enrolled in the NCT03340935 trial completed an average of 5.4 FMD cycles, out of the maximum number of 8 cycles allowed per protocol), which is in line with data previously published in the whole study cohort. During each FMD cycle patients underwent a reduction in their BMI (mean reduction: 4.0 percent), which was partially recovered during the refeeding, and finally stabilized after the fifth FMD cycle (Figure S1). Plasma glucose, insulin and IGF-1 concentrations were significantly reduced, and urinary ketones were significantly increased, during each FMD cycle, Figure S2. These data are consistent with metabolic modifications previously reported in the whole NCT trial patient cohort.
Section Three point two. Antitumor activity and efficacy of cyclic FMD in combination with CBDCA-based chemotherapy.
Median follow-up was 44.0 months (95percent Confidence Interval: 40.3-NR) for patients treated with chemotherapy plus FMD in the context of the NCT trial, while it was 52.1 months (95 percent Confidence Interval: 50.2-NR) in the control cohort.
Patients undergoing cyclic FMD experienced significantly longer OS as compared to patients in the control cohort (median OS: 30.3 months, 95percent Confidence Interval: 18-NR, versus 17.2 months, 95 percent Confidence Interval: 15.3 to 25.1, respectively; log-rank P value: .041; Figure 2A). At univariate analysis, covariates associated with lower OS were ECOG PS (ECOG PS 1 versus 0: HR 2.42, 95percent Confidence Interval: 1.37 to 4.28, P equals .002), higher number of metastatic sites, greater than 3 versus 1 to 3: HR 2.03, 95percent Confidence Interval: 1.28 to 3.23, P equals .003) and presence of lung metastases, yes versus no: HR 1.69, 95percent Confidence Interval: 1.0 to 2.67, P equals .024; Table 2. Patients with liver or visceral metastases showed a trend toward worse OS (HR 1.60, 95percent Confidence Interval: 0.96-2.66, P equals .071 and HR 1.61, 95percent Confidence Interval: 1.00 to 2.59, P equals .051, respectively). When the association between FMD administration and clinical outcomes was adjusted for these covariates, FMD use remained significantly and independently associated with better patient OS (HR 0.4, 95percent Confidence Interval: 0.19 to 0.86, P equals .019; Table 3). Importantly, this OS advantage was confirmed at both univariate and multivariable analysis after propensity scorebased matching of patients according to ECOG PS, meaning, the only other clinical characteristic, together with FMD use, which maintained an independent association with patient OS at multivariable analysis) and the presence of de novo metastatic disease, meaning, the only characteristic that was highly unbalanced between the two treatment groups; Figure 3A and Table S1).
FMD use was also associated with independently better OS in a multivariable Cox regression model including a higher number of covariates that were selected by using a less stringent threshold for statistical significance, P less than 0.1, based on univariate analyses, namely ECOG PS, visceral metastases, liver metastases, lung metastases and number of metastatic sites (Table S2).
Regarding PFS outcomes, we found no significant PFS differences between patients treated with or without FMD (median PFS: 7.09 months, 95 percent Confidence Interval: 4.01-NR, versus 6.61 months, 95 percent Confidence Interval: 5.30 to 8.95; log-rank test P value equals .3; Figure S3A), while patients with a higher number of metastatic sites, greater than 3 versus 1 to 3, had worse PFS (HR 1.8, 95 percent Confidence Interval: 1.16 to 2.79, P equals .009; Table S3). Of note, after propensity score matching, patients receiving FMD showed a trend toward better PFS when compared to patients not undergoing FMD (Figure 3B).
Among patients receiving cyclic FMD, 14.3 percent, 57.1 percent, 7.14 percent and 21.4 percent of patients obtained complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD) as their best tumor response, respectively, as compared to 9.2 percent, 47.4 percent, 22.4 percent and 21.0 percent of patients in the control group, respectively (Figure S4A). We found no statistically significant different ORR or DCR between patients receiving or not receiving FMD (ORR: 71.4 percent versus 56.6 percent, P equals .46; DCR: 78.6 percent versus 78.9 percent, P equals 1, respectively; Figure S4B, C).
Section Three point three. Subgroup analysis in patients treated with first-line CBDCA-gemcitabine
We recently published the results of a retrospective study, which showed that, among aTNBC patients pretreated with taxanes in the context of neo adjuvant chemotherapy, those receiving first-line CBDCA-gemcitabine have better PFS and OS when compared to patients receiving first-line CBDCA-paclitaxel.
TABLE One. Patient and tumor characteristics. The overall, FMD and P-Values are given.
Figure Two in text. Overall survival probability in aTNBC patients treated with CBDCA-based chemotherapy receiving and not receiving FMD.
Kaplan-Meier curves representing OS of the whole study cohort (A) and of the subgroup of patients receiving CBDCA in combination with gemcitabine (B).
TABLE Two in text. Univariate Cox proportional model for OS, Variables and the Hazard rations, Confidence interval and P-Values are listed.
In the present study, all patients, 100 percent, undergoing cyclic FMD in combination with platinum-based chemotherapy received CBDCA-gemcitabine as chemotherapy backbone, while only 25 percent of patients in the control cohort received this chemotherapy regimen.
To exclude that an imbalance in the type of chemotherapy regimen could account for the observed OS advantage in patients receiving FMD in combination with chemotherapy, we compared the OS in patients receiving CBDCA plus gemcitabine plus FMD with the OS of a subcohort of control patients treated with CBDCA plus gemcitabine.
The characteristics of this patient subcohort are summarized in Table S4. Patients treated with FMD in combination with CBDCA-gemcitabine showed a trend toward better OS when compared to patients receiving CBDCA-gemcitabine alone, median OS: 30.3 months, 95 percent Confidence Interval: 18.0-NR, versus 15.3 months, 95 percent Confidence Interval 13.7 to31.6, log-rank P value equals .052; Figure 2B).
The only other clinical characteristic associated with OS was ECOG PS (HR 3.03, 95 percent Confidence Interval 1.28 to 7.16, P value equals .012; Table S5). Importantly, when we fitted a bivariate Cox regression model including FMD and ECOG PS, the FMD maintained an independent and statistically significant association with better patient OS (Table S6). Similar to what was observed in the whole control cohort, we found no significant PFS differences between patients receiving CBDCA-gemcitabine or CBDCA gemcitabine-FMD (Figure S3B).
Three point four. Short and long-term impact of FMD on plasmatic glucose levels.
Given the acknowledged mechanistic role of FMD-induced reduction of blood glucose concentration in mediating FMD antitumor effects in TNBC preclinical models we evaluated plasmatic glucose levels in patients receiving FMD in combination with chemotherapy, as well as in the control population of patients receiving chemotherapy alone.
Patients receiving experimental FMD in combination with carboplatin-based chemotherapy underwent an acute reduction of plasma glucose concentration at the end of each FMD cycle (Figure S1A), thus recapitulating data previously published by our group in the whole NCT03340935 trial cohort.
Interestingly, patients undergoing FMD also had chronically lowered blood glucose concentration as compared to patients receiving chemotherapy alone, thus indicating a potential carry over effect of the FMD in terms of lowering blood glucose levels also during the refeeding intervals (Figure S5). These results indicate that patients undergoing cyclic FMD are exposed to lower systemic blood glucose concentration, and that their tumors could be exposed to overall lower extracellular glucose levels over the time.
Of note, in the whole study cohort, which included both patients treated with FMD and patients in the control cohort, higher baseline glycemia was associated with significantly worse patient OS, thus confirming previous data published by our group in a cohort of aTNBC patients partially overlapping with the population of patients included in the present study.
Four. DISCUSSION.
We showed that aTNBC patients undergoing cyclic FMD in combination with first-line CBDCA-gemcitabine chemotherapy have better OS when compared to aTNBC patients treated with CBDCA-gemcitabine or CBDCA-paclitaxel without the FMD. The OS benefit observed in
FMD-treated patients was maintained after adjustment for established prognostic covariates, such as patient ECOG PS, the number of metastatic sites and the presence of metastases in the lung, which were also associated with worse OS in our study.
FIGURE Three in Text. Overall survival (OS) and progression-free survival (PFS) after propensity score matching. Kaplan-Meier curves representing (A) OS and (B) PFS in aTNBC patients treated with CBDCA-based chemotherapy in combination with FMD and in a matched cohort of aTNBC patients treated with CBDCA-based chemotherapy alone. Patients were selected with propensity score matching according to ECOG PS and the presence of de novo metastatic disease.
TABLE Three in text. Multivariable Cox proportional model for OS.
Despite the OS benefit observed in patients undergoing chemotherapy plus FMD, we did not observe PFS differences between these clinical cohorts. The discrepancy between OS and PFS findings can be explained by several factors. First, the FMD might not improve tumor response to chemotherapy, but it could favor long-term tumor growth control by boosting antitumor immune responses. This interpretation is supported by previously published preclinical studies, which showed that fasting, FMD-induced boost in antitumor immunity is crucial to mediate its antitumor effects, and by our clinical findings showing that the FMD promotes the cytotoxic activity of immune cell populations, such as CD8 plus T cells, NK cells and memory T cells, at both systemic and tumor levels, in breast cancer patients. Based on these preclinical and clinical data, the observed OS advantage in aTNBC patients receiving chemotherapy plus FMD could result from FMD-induced boost of systemic antitumor immunity which, in turn, may produce long-lasting activation of the immune system and long term tumor control also in the absence of a short-term clinical benefit, ORR, PFS.
One potentially alternative explanation to the study findings is that patients enrolled in the NCT trial initiated the experimental treatment between February 2017 and February 2020, that is, more recently than patients included in the control cohort. Since several new and effective drugs have been included in the therapeutic armamentarium for aTNBC patients in recent years, such as immune checkpoint inhibitors, Sacituzumab-govitecan, trastuzumab deruxtecan for patients with HER2-low TNBC, or PARP inhibitors in patients with germline BRCA1, BRCA2 mutations, we performed additional analyses to evaluate whether patients undergoing cyclic FMD received a higher average number of subsequent lines of systemic therapy after progressing on first-line CBDCA-based chemotherapy.
Actually, the average number of subsequent lines of systemic treatment in the FMD cohort was 1.64, while it was 1.85 in the control cohort. A recent preclinical study conducted in mouse TNBC models showed that cyclic FMD reduces TNBC CSCs by lowering glucose concentration in the extracellular environment, and that the anti-CSC activity of the FMD is essential to mediate its antitumor effects. In the present study, we found that aTNBC patients undergoing cyclic FMD in combination with chemotherapy experience an acute reduction of blood glucose during each FMD cycle, and that they are also exposed to globally lower plasmatic glucose concentrations during the treatment when compared to patients receiving chemotherapy alone.
As we also showed that higher plasmatic glucose levels are associated with worse aTNBC patient outcomes, in line with a solid body of preclinical evidence, FMD-mediated acute and chronic reduction of plasmatic glucose levels could explain the observed better survival of patients receiving FMD.
Future prospective studies in larger patient populations will clarify if adding cyclic FMD to standard anticancer treatments improves clinical outcomes in TNBC patients. In this respect, in June 2020 we initiated a phase two, randomized clinical study, namely the “BREAKFAST” trial, NCT-04-24-89-98, to investigate if adding cyclic FMD to standard anthracycline-taxane chemotherapy improves pathologic complete tumor responses when compared to chemotherapy alone. However, our study has been precociously interrupted due to changes in the standard-of-care therapy of stage two, three TNBC, which now includes the anti-PD1 monoclonal antibody pembrolizumab in combination with anthracycline-taxane-CBDCA chemotherapy. Therefore, we recently initiated a new phase two trial, namely the multicentric, randomized “BREAKFAST 2” study, NCT 05-76-39-92, which will investigate if cyclic FMD in addition to standard neoadjuvant chemoimmunotherapy improves pCR rates as compared to chemoimmunotherapy alone in patients with stage two to threeTNBC. Among secondary endpoints of the BREAKFAST 2 study are disease-free survival (DFS) and OS. Therefore, the BREAKFAST 2 trial may provide more convincing evidence that adding cyclic FMD to standard treatments can improve their antitumor activity, efficacy in patients with early stage TNBC.
The main limitations of the current study consist of the low number of patients undergoing cyclic FMD in combination with CBDCAgemcitabine chemotherapy, as well as in the lack of randomization procedures to assign patients to chemotherapy or chemotherapy plus FMD. These limitations preclude the possibility to draw strong conclusions about the positive impact of the FMD on clinical outcomes.
However, the observed clinical findings are promising, and they are in line with a considerable body of preclinical literature showing strong antitumor effects of cyclic fasting, FMD in combination with chemotherapy, including platinum-based chemotherapy, immunotherapy or other treatments specifically in TNBC models. Future, randomized controlled trials with appropriate sample size and power, such as the ongoing BREAKFAST-2 study, will clarify if adding cyclic FMD to standard chemotherapy or chemoimmunotherapy is able to improve clinical outcomes in patients with early-stage or advanced TNBC.
Another limitation of our study consists in the fact that most patients had not received neoadjuvant CBDCA-based chemotherapy, which is now part of the standard-of-care neoadjuvant therapy for stage two, three TNBC patients. In particular, we do not know if results of our study also apply to patients relapsing after exposure to more effective systemic therapies, such as neoadjuvant anthracycline-taxane-CBDCA chemotherapy plus pembrolizumab. Finally, patients included in our study were not evaluated for tumor PD-L1 status, and none of them received immune checkpoint inhibitors as part of their first-line therapy. Therefore, we do not know if adding cyclic FMD to first-line chemo immunotherapy in patients with PD-L1-positive disease may also add clinical benefit when compared to chemoimmunotherapy alone.
In conclusion, our study provides first clinical evidence that combining cyclic FMD with standard first-line CBDCA-based chemotherapy could improve OS in aTNBC patients. These results are in line with a large body of preclinical data consistently showing that cyclic fasting and FMD improve the antitumor efficacy of chemotherapy, targeted therapies and immunotherapy in TNBC models, and that the positive immunomodulatory effects of fasting, FMD are essential to produce these antitumor effects.
Our study paves the way for further investigation of cyclic FMD in combination with first-line chemotherapy or chemoimmunotherapy in patients with PD-L1-negative or PD-L1-positive aTNBC, respectively.
AUTHOR CONTRIBUTIONS, ACKNOWLEDGEMENTS, CONFLICT OF INTEREST STATEMENT, ETHICS STATEMENT and References.
-

BonginoReport
3 hours agoSuper Bowl Vibe Shift: Trump Cheered, Taylor Swift Booed (Ep.136) - 02/10/2025
29K36 -
 LIVE
LIVE
Wendy Bell Radio
4 hours agoThe Rats Are Scrambling
13,024 watching -
 LIVE
LIVE
Jeff Ahern
1 hour agoMonday Madness with Jeff Ahern (put a fork in them)
713 watching -

Dad Dojo Podcast
7 hours ago $0.35 earnedEP19: Cashing In Crypto
5.61K -
 2:30:07
2:30:07
TheDozenPodcast
20 hours agoEpstein island, fake news, Royal Family scandal: Dan Wootton
3.63K1 -
![RASKIN THREATENS CLASS ACTION TO STOP MUSK. BERNIE LIES TO THE PUBLIC ABOUT DOGE [EP 4434-8AM]](https://1a-1791.com/video/fwe1/5e/s8/1/_/a/t/I/_atIx.0kob-small-RASKIN-THREATENS-CLASS-ACTI.jpg) LIVE
LIVE
The Pete Santilli Show
3 hours agoRASKIN THREATENS CLASS ACTION TO STOP MUSK. BERNIE LIES TO THE PUBLIC ABOUT DOGE [EP 4434-8AM]
1,563 watching -
 10:31
10:31
Space Ice
22 hours agoHardcore Henry - A Average Day In The Life Of Space Ice - Best Movie Ever
5.28K22 -
 8:03
8:03
Colion Noir
21 hours agoA Judge Just Ruled You Can Own A Machine Gun
14.5K53 -
 46:13
46:13
Survive History
22 hours ago $0.49 earnedCould You Survive in the Roman Special Forces?
8.28K -
 19:40
19:40
Fit'n Fire
22 hours ago $0.02 earnedThe Best PDW -- Sig Sauer MPX 8" PDW
4.34K4