Premium Only Content
Excess mortality in the Western World since COVID-19. Saskia Mostert. A Puke (TM) Audiopaper
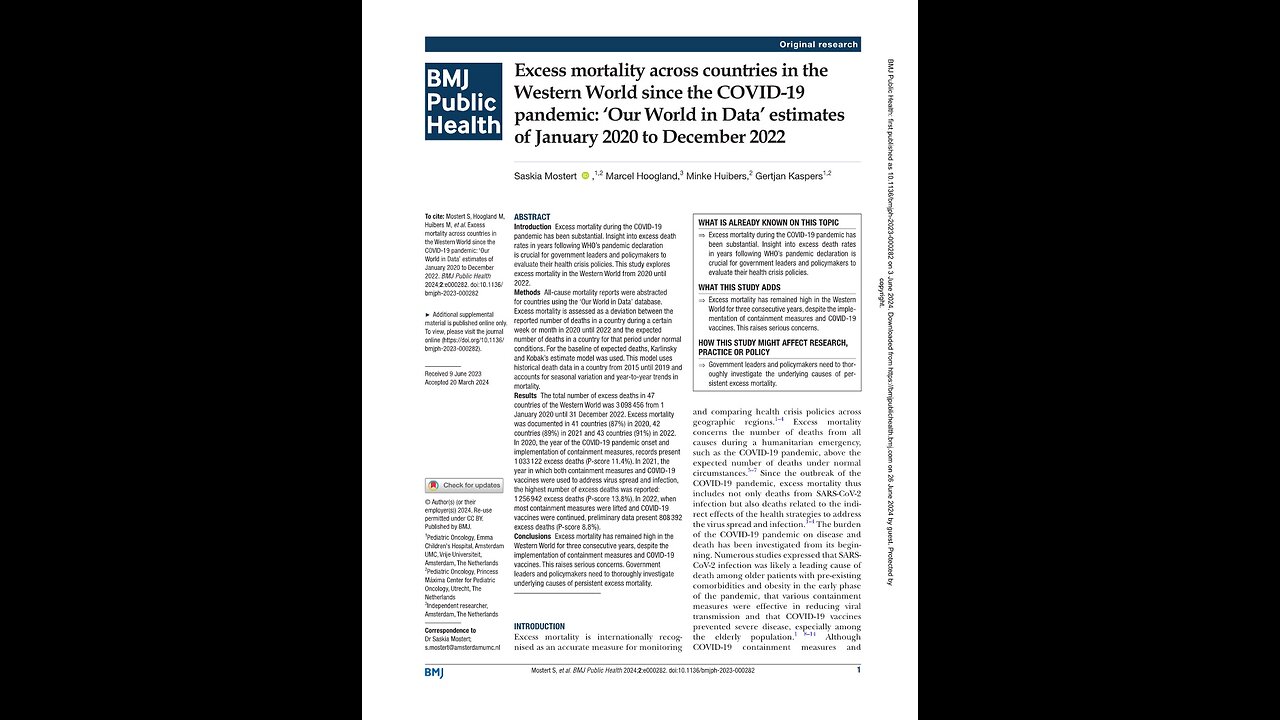
Excess mortality across countries in the Western World since the COVID-19 pandemic: Our World in Data estimates of January 2020 to December 2022.
Mostert S, et al. BMJ Public Health 2024;2:e000282. doi:10.1136/bmjph-2023-000282
doi:10.1136/ bmjph-2023-00028
https://bmjpublichealth.bmj.com/content/bmjph/2/1/e000282.full.pdf
Correspondence to Dr Saskia Mostert.
s.mostert@amsterdamumc.nl
Excess mortality across countries in the Western World since the COVID-19 pandemic.
Saskia Mostert and others.
Received 9 June 2023. Accepted 20 March 2024
ABSTRACT.
Introduction Excess mortality during the COVID-19 pandemic has been substantial. Insight into excess death rates in years following WHO’s pandemic declaration is crucial for government leaders and policymakers to evaluate their health crisis policies. This study explores excess mortality in the Western World from 2020 until 2022.
Methods.
All-cause mortality reports were abstracted for countries using the Our World in Data database. Excess mortality is assessed as a deviation between the reported number of deaths in a country during a certain week or month in 2020 until 2022 and the expected number of deaths in a country for that period under normal conditions. For the baseline of expected deaths, Karlinsky and Kobak’s estimate model was used. This model uses historical death data in a country from 2015 until 2019 and accounts for seasonal variation and year-to-year trends in mortality.
Results.
The total number of excess deaths in 47 countries of the Western World was 3,098,456 from 1 January 2020 until 31 December 2022. Excess mortality was documented in 41 countries (87 percent) in 2020, 42 countries (89 percent) in 2021 and 43 countries (91 percent) in 2022. In 2020, the year of the COVID-19 pandemic onset and implementation of containment measures, records present 1,033,122 excess deaths (P-score 11.4 percent). In 2021, the year in which both containment measures and COVID-19 vaccines were used to address virus spread and infection, the highest number of excess deaths was reported: 1,256,942 excess deaths (P-score 13.8 percent). In 2022, when most containment measures were lifted and COVID-19 vaccines were continued, preliminary data present 808 392 excess deaths, P-score 8.8 percent.
Conclusions.
Excess mortality has remained high in the Western World for three consecutive years, despite the implementation of containment measures and COVID-19 vaccines. This raises serious concerns. Government leaders and policymakers need to thoroughly investigate underlying causes of persistent excess mortality.
What is already known on this topic.
Excess mortality during the COVID-19 pandemic has been substantial. Insight into excess death rates in years following WHO’s pandemic declaration is crucial for government leaders and policymakers to evaluate their health crisis policies.
What this study adds.
Excess mortality has remained high in the Western World for three consecutive years, despite the implementation of containment measures and COVID-19 vaccines. This raises serious concerns.
How this study might affect research, practice or policy.
Government leaders and policymakers need to thoroughly investigate the underlying causes of persistent excess mortality.
Introduction.
Excess mortality is internationally recognised as an accurate measure for monitoring and comparing health crisis policies across geographic regions. Excess mortality concerns the number of deaths from all causes during a humanitarian emergency, such as the COVID-19 pandemic, above the expected number of deaths under normal circumstances. Since the outbreak of the COVID-19 pandemic, excess mortality thus includes not only deaths from SARS-CoV-2 infection but also deaths related to the indirect effects of the health strategies to address the virus spread and infection. The burden of the COVID-19 pandemic on disease and death has been investigated from its beginning. Numerous studies expressed that SARS CoV-2 infection was likely a leading cause of death among older patients with pre-existing comorbidities and obesity in the early phase of the pandemic, that various containment measures were effective in reducing viral transmission and that COVID-19 vaccines prevented severe disease, especially among the elderly population.
Although COVID-19 containment measures and COVID-19 vaccines were thus implemented to protect citizens from suffering morbidity and mortality by the COVID-19 virus, they may have detrimental effects that cause inferior outcomes as well. It is noteworthy that excess mortality during a crisis points to a more extensive underlying burden of disease, disablement and human suffering. On 11 March 2020, WHO declared the COVID-19 pandemic. Countries in the Western World promptly implemented COVID-19 containment measures, such as lockdowns, school closures, physical distancing, travel restrictions, business closures, stay-at-home orders, curfews and quarantine measures with contact tracing, to limit virus spread and shield its residents from morbidity and mortality. These non-pharmaceutical interventions however had adverse indirect effects, such as economic damage, limited access to education, food insecurity, child abuse, limited access to healthcare, disrupted health programmes and mental health challenges, that increased morbidity and mortality from other causes. Vulnerable populations in need of acute or complex medical treatment, such as patients with cardiovascular disease, cerebrovascular conditions, diabetes and cancer, were hurt by these interventions due to the limited access to and delivery of medical services. Shortage of staff, reduced screening, delayed diagnostics, disrupted imaging, limited availability of medicines, postponed surgery, modified radiotherapy and restricted supportive care hindered protocol adherence and worsened the condition and prognosis of patients. A recent study investigated excess mortality from some major non-COVID causes across 30 countries in 2020. Significant excess deaths were reported from ischaemic heart diseases (in 10 countries), cerebrovascular diseases (in 10 countries) and diabetes (in 19 countries).
On 14 October 2020, Professor Ioannidis from Stanford University published an overall Infection Fatality Rate of COVID-19 of 0.23 percent, and for people aged less than 70 years, the Infection Fatality Rate was 0.05 percent. Governments in the Western World continued to impose lockdowns until the end of 2021. In December 2020, the UK, the USA and Canada were the first countries in the Western World that started with the roll-out of the COVID-19 vaccines under emergency authorisation.
At the end of December 2020, a large randomised and placebo-controlled trial with 43548 participants was published in the New England Journal of Medicine, which showed that a two-dose mRNA COVID-19 vaccine regimen provided an absolute risk reduction of 0.88 percent and relative risk reduction of 95 percent against laboratory-confirmed COVID-19 in the vaccinated group.
Or 8 COVID-19 cases out of 17,411 vaccine recipients, versus the placebo group, 162 COVID-19 cases, 17,511 placebo recipients. At the beginning of 2021, most other Western countries followed with rolling out massive vaccination campaigns. On 9 April 2021, the overall COVID-19 Infection Fatality Rate was reduced to 0.15 percent and expected to further decline with the widespread use of vaccinations, prior infections and the evolution of new and milder variants.
Although COVID-19 vaccines were provided to guard civilians from suffering morbidity and mortality by the COVID-19 virus, suspected adverse events have been documented as well. The secondary analysis of the placebo-controlled, phase III randomised clinical trials of mRNA COVID-19 vaccines showed that the Pfizer trial had a 36 percent higher risk of serious adverse events in the vaccine group. The risk difference was 18.0 per 10 000 vaccinated 95 percent Confidence Interval, C I, of 1.2 to 34.9, and the risk ratio was 1.36 (95 percent CI 1.02 to 1.83). The Moderna trial had a 6 percent higher risk of serious adverse events among vaccine recipients. The risk difference was 7.1 per 10,000 vaccinated (95 percent CI 23.2 to 37.4), and the risk ratio was 1.06 (95 percent CI 0.84 to 1.33).
By definition, these serious adverse events lead to either death, are life-threatening, require inpatient (prolongation of) hospitalisation, cause persistent, significant disability, incapacity, concern a congenital anomaly, birth defect or include a medically important event according to medical judgement. The authors of the secondary analysis point out that most of these serious adverse events concern common clinical conditions, for example, ischaemic stroke, acute coronary syndrome and brain haemorrhage. This commonality hinders clinical suspicion and consequently its detection as adverse vaccine reactions. Both medical professionals and citizens have reported serious injuries and deaths following vaccination to various official databases in the Western World, such as VAERS in the USA, Eudra Vigilance in the European Union and Yellow Card Scheme in the UK. A study comparing adverse event reports to VAERS and EudraVigilance following mRNA COVID-19 vaccines versus influenza vaccines observed a higher risk of serious adverse reactions for COVID-19 vaccines. These reactions included cardiovascular diseases, coagulation, haemorrhages, gastrointestinal events and thromboses.
Numerous studies reported that COVID-19 vaccination may induce myocarditis, pericarditis and autoimmune diseases. Post mortem examinations have also ascribed myocarditis, encephalitis, immune thrombotic thrombocytopenia, intracranial haemorrhage and diffuse thrombosis to COVID-19 vaccinations. The Food and Drug Administration noted in July 2021 that the following potentially serious adverse events of Pfizer vaccines deserve further monitoring and investigation: pulmonary embolism, acute myocardial infarction, immune thrombocytopenia and disseminated intravascular coagulation. Insight into the excess death rates in the years following the declaration of the pandemic by WHO is crucial for government leaders and policymakers to evaluate their health crisis policies. This study therefore explores excess mortality in the Western World from 1 January 2020 until 31 December 2022.
MATERIALS AND METHODS.
Setting.
The Western World is primarily defined by culture rather than geography. It refers to various countries in Europe and to countries in Australasia, Australia, New Zealand, and North America (the USA, Canada) that are based on European cultural heritage. The latter countries were once British colonies that acquired Christianity and the Latin alphabet and whose populations comprised numerous descendants from European colonists or migrants.
Study design.
All-cause mortality reports were abstracted for countries of the Western World using the Our World in Data database. Only countries that had all-cause mortality reports available for all three consecutive years, 2020 to 2022, were included. If coverage of one of these years was missing, the country was excluded from the analysis. The Our World in Data database retrieves their reported number of deaths from both the Human Mortality Database (HMD) and the World Mortality Dataset (WMD). HMD is sustained by research teams of both the University of California in the USA and the Max Planck Institute for Demographic Research in Germany. HMD recovers its data from Eurostat and national statistical agencies on a weekly basis. The Our World in Data database used HMD as their only data source until February 2021.
WMD is sustained by the researchers Karlinsky and Kobak. WMD recovers its data from HMD, Eurostat and national statistical agencies on a weekly basis. The Our World in Data database started to use WMD as a data source next to HMD since February 2021.
Excess mortality is assessed as the deviation between the reported number of deaths in a country during a certain week or month in 2020 until 2022 and the expected or projected number of deaths in a country for that period under normal conditions.
For the baseline of expected deaths, the estimate model of Karlinsky and Kobak was used. This linear regression model uses historical death data in a country from 2015 until 2019 and accounts for seasonal variation in mortality and year to year trends due to changing population structure or socioeconomic factors.
Karlinsky and Kobak fit their regression model separately for every country:
D t, Y equals alpha t plus betas times Y plus epsilon.
In this formula, D t, Y is the number of deaths observed on week (or month) t in year Y, beta is a linear slope across years, alpha t are separate intercepts (fixed effects) for each week (month, quarter) and epsilon, effectively N (zero, sigma squared) is the Gaussian noise.
The model prediction for 2020 is taken as the baseline for the excess mortality calculations:
B ¬t equals alpha ¬t plus beta times 2020.
The final excess mortality estimate is as follows:
Sum over t greater than, or equal to t 1 of D t, 2020 minus B t plus.
The sum over t of D t, 2021 minus B t.
Where t 1 indicates the summation onset in 2020. The variance Var (Of delta) of estimator delta is computed as follows: X is the predictor matrix in the regression, y is the response vector,
Beta equals the inverse of the matrix X transpose X, times X transpose y, and is the vector of estimated regression coefficients, and
Sigma squared equals the two norm of y minus X times beta, divided by n minus p is the unbiased estimate of noise variance, in which n is the sample size and P is the number of predictors.
The covariance of beta equals sigma squared times the inverse of X transpose X, and is the covariance matrix of beta.
S equals Covariance of Beta t equals Covariance of X 2020 times Beta equals sigma squared X 2020 times the inverse of X transpose X times X 2020 transpose, is the covariance matrix of predicted baseline values beta t, where X 2020 is the predictor matrix for 2020.
Karlinsky and Kobak depict vector w with elements w t of length equal to the number of rows in X 2020. They set all elements before t 1 to zero, all elements from t 1 forward to 1, and raise by one all elements corresponding to 2021 data.
The predictive variance of delta is denoted as follows:
Variance of Delta equals Variance of the sum over t of w t B t plus the sum over t of w t times sigma squared, which equals:
W transpose S w plus sigma squared times the norm of W.
In which the first term represents the uncertainty of Beta t and the second term represents the additive Gaussian noise. The square root of the Variance of Delta is regarded as the standard error of delta.
When the fraction z equals absolute value of delta over the square root of the variance of delta is below 2, the excess mortality of that country is considered not significantly different from zero.
The model regards excess mortality during the COVID-19 pandemic as the sum of the following factors:
(a) Deaths directly generated by SARS-CoV-2 infection,
(b) Deaths generated by medical system overload owing to the pandemic,
(c) Excess deaths from other natural causes, for example, influenza and other infectious respiratory diseases during winter seasons,
(d) Excess deaths from unnatural causes, for example, traffic accidents, homicides, suicides, deaths from drug overdoses and unintentional injuries, and,
(e) Excess deaths from extreme events, such as heat waves, wars, power outages and natural disasters.
Karlinsky and Kobak’s model expressly takes factor (e) into account and acknowledges that the contribution of factors (b), (c) and (d) is in general minor for the majority of nations compared with factor (a).
The researchers have used the officially reported national COVID-19 death counts from the WHO dataset. In their model, common seasonal influenza during 2015 and 2019 contributes to the projected baseline of expected deaths.
In addition, the model corrects for peaks of excess deaths during heat waves.
Because the number of excess deaths is impacted by the population size of a nation, the excess mortality estimates have been normalized by the population size. Population size estimates of the United Nations World Population Prospect dataset have been used to estimate excess deaths per 100000 population for 2020 until 2022. Because the Infection Fatality Rate of SARS-CoV-2 is age dependent and nations have different age structures, the excess mortality estimates have been normalized by the yearly sum of the baseline mortality to account for the nation’s age structure.
Because the projected baseline uses a linear trend, the model can also reckon for ameliorations in death registration across recent years.
For each country separately, Karlinsky and Kobak have taken these various factors into account when predicting the baseline mortality for 2020 until 2022. If required, adjustments have been made accordingly.
For example, in the USA, the weekly death data, with R squared equals 0.89, F equals 31.7, give rise to the following: beta equals 773 plus or minus 57. This implies that every year, the number of weekly deaths rises on average by around 800. The predicted weekly deaths for 2020 are thus higher than the 2015 to 2019 average. Regarding the strong and statistically significant annual trend, it is therefore not accurate to employ the 2015 to 2019 data as a baseline. Another example of correction concerns Belgium, the Netherlands, France, Luxembourg and Germany. In August 2020, a peak of excess deaths was observed during a heat wave in these countries. To account for this, weeks 32 to 34 were excluded from the excess mortality calculation in these nations. This decreased the excess mortality estimates for these countries by 1500 for Belgium, 660 for the Netherlands, 1600 for France, 35 for Luxembourg and 3700 for Germany.
Karlinsky and Kobak present more details about the used method in their joint publication. Excess mortality P-score concerns the percentage difference between the reported number of deaths and the projected number of deaths in a country. This measure permits comparisons between various countries. Although presenting the raw number of excess deaths provides insight into the scale, it is less useful to compare countries because of their large population size variations.
The Our World in Data’ database presents P-scores in a country during a certain week or month in 2020 until 2022. These P-scores are calculated from both the reported number of deaths in HMD and WMD and the projected number of deaths using the estimate model of Karlinsky and Kobak in WMD.
For correct interpretation of excess mortality provided by the Our World in Data database, the following needs to be taken into consideration: the reported number of deaths may not represent all deaths, as countries may lack the infrastructure and capacity to document and account for all deaths. In addition, death reports may be incomplete due to delays. It may take weeks, months or years before a death is actually reported. The date of a reported death may refer to the actual death date or to its registration date. Sometimes, a death may be recorded but not the date of death. Countries that provide weekly death reports may use different start and end dates of the week. Most countries define the week from Monday until Sunday, but not all countries do. Weekly and monthly reported deaths may not be completely comparable, as excess mortality derived from monthly calculations inclines to be lower. For our analysis, weekly all-cause mortality reports from the Our World in Data database were converted to monthly reports. Subsequently, the monthly reports were converted to annual reports.
Patient and public involvement.
Patients and, or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
RESULTS.
The Our World in Data database contained all-cause mortality reports of 47 countries (96 percent) in the Western World for the years 2020, 2021 and 2022. Only Andorra and Gibraltar were excluded. Both countries lacked all-cause mortality reports for the year 2022. Most countries (n equals 36, 77 percent) present weekly all-cause mortality reports, whereas 11 countries (23 percent) report monthly. The latter countries include the following: Albania, Bosnia Herzegovina, Faeroe Islands, Greenland, Kosovo, Liechtenstein, Moldova, Monaco, North Macedonia, San Marino and Serbia. The all-cause mortality reports were abstracted from the Our World in Data database on 20 May 2023. At this date, four countries (9 percent) still lacked all-cause mortality reports for various periods: Canada (1 month), Liechtenstein (3 months), Monaco (3 months) and Montenegro (4 months). It is noteworthy that all-cause mortality reports are also still being updated for the other countries due to registration delays which may take weeks, months or even years.
Excess mortality.
Online supplemental table 1 illustrates that the total number of excess deaths in the 47 countries of the Western World was 3,098,456 from 1 January 2020 until 31 December 2022.
Excess mortality was documented in 41 countries (87 percent) in 2020, in 42 countries (89 percent) in 2021 and in 43 countries (91 percent) in 2022.
In 2020, the year of the COVID-19 pandemic and implementation of the containment measures, 1,033,122 excess deaths (P-score 11.4 percent) were recorded. In 2021, the year in which both COVID-19 containment measures and COVID-19 vaccines were used to address virus spread and infection, a total of 1,256,942 excess deaths (P-score 13.8 percent) were reported. In 2022, the year in which most containment measures were lifted and COVID-19 vaccines were continued, preliminary available data counts 808392 excess deaths (P-score 8.8 percent).
Figure 1 presents the excess mortality and cumulative excess mortality in 47 countries of the Western World over the years 2020, 2021 and 2022.
The linear excess mortality trendline is almost horizontal.
Excess mortality P-scores.
Figure 2 shows the excess mortality P-scores per country in the Western World. Only Greenland had no excess deaths between 2020 and 2022. Among the other 46 countries with reported excess mortality, the percentage difference between the reported and projected number of deaths was highest in 13 countries (28 percent) during 2020, in 21 countries (46 percent) during 2021 and in 12 countries (26 percent) during 2022.
Figure 3 exemplifies excess mortality P-score curves of the highest-populated country of North America (the USA), the four highest-populated countries of Europe (Germany, France, the UK and Italy) and the highest-populated country of Australasia (Australia).
Figure 4 highlights a map of excess mortality P-scores in the Western World over the years 2020, 2021 and 2022.
Table 1 presents a classification of excess mortality P-scores in the Western World.
DISCUSSION.
This study explored the excess all-cause mortality in 47 countries of the Western World from 2020 until 2022. The overall number of excess deaths exceeded three million. Excess mortality was registered in 87 percent of countries in 2020, in 89 percent of countries in 2021 and in 91 percent of countries in 2022. During 2020, which was marked by the COVID-19 pandemic and the onset of mitigation measures, one million excess deaths (P-score 11.4 percent) were to be regretted. A recent analysis of sero prevalence studies in this prevaccination era illustrates that the Infection Fatality Rate estimates in non-elderly populations were even lower than prior calculations suggested. At a global level, the pre vaccination Infection Fatality Rate was 0.03 percent for people aged less than 60 years and 0.07 percent for people aged less than 70 years.
For children aged zero to nineteen years, the Infection Fatality Rate was set at 0.0003 percent.
This implies that children are rarely harmed by the COVID-19 virus. During 2021, when not only containment measures but also COVID-19 vaccines were used to tackle virus spread and infection, the highest number of excess deaths was recorded:
One and a quarter million excess deaths (P-score 13.8 percent). Scientific consensus regarding the effectiveness of non-pharmaceutical interventions in reducing viral transmission is currently lacking. During 2022, when most mitigation measures were negated and COVID-19 vaccines were sustained, preliminary available data count eight hundred thousand excess deaths (P-score 8.8 percent).
The percentage difference between the documented and projected number of deaths was highest in 28 percent of countries during 2020, in 46 percent of countries during 2021, and in 26 percent of countries during 2022.
This insight into the overall all-cause excess mortality since the start of the COVID-19 pandemic is an important first step for future health crisis policy decision-making.
The next step concerns distinguishing between the various potential contributors to excess mortality, including COVID-19 infection, indirect effects of containment measures and COVID-19 vaccination programmes. Differentiating between the various causes is challenging. National mortality registries not only vary in quality and thoroughness but may also not accurately document the cause of death.
The usage of different models to investigate cause-specific excess mortality within certain countries or subregions during variable phases of the pandemic complicates elaborate cross-country comparative analysis. Not all countries provide mortality reports categorized per age group. Also testing policies for COVID-19 infection differ between countries. Interpretation of a positive COVID-19 test can be intricate. Consensus is lacking in the medical community regarding when a deceased infected with COVID-19 should be registered as a COVID-19 death.
Indirect effects of containment measures have likely altered the scale and nature of disease burden for numerous causes of death since the pandemic. However, deaths caused by restricted healthcare utilisation and socioeconomic turmoil are difficult to prove. A study assessing excess mortality in the USA observed a substantial increase in excess mortality attributed to non-COVID causes during the first 2 years of the pandemic. The highest number of excess deaths was caused by heart disease, 6 percent above base-line during both years. Diabetes mortality was 17 percent over baseline during the first year and 13 percent above it during the second year. Alzheimer’s disease mortality was 19 percent higher in year 1 and 15 percent higher in year 2. In terms of percentage, large increases were recorded for alcohol related fatalities (28 percent over baseline during the first year and 33 percent during the second year) and drug-related fatalities (33 percent above baseline in year 1 and 54 percent in year 2).
Previous research confirmed profound under-reporting of adverse events, including deaths, after immunisation. Consensus is also lacking in the medical community regarding concerns that mRNA vaccines might cause more harm than initially forecasted. French studies suggest that COVID-19 mRNA vaccines are gene therapy products requiring long-term stringent adverse events monitoring. Although the desired immunisation through vaccination occurs in immune cells, some studies report a broad biodistribution and persistence of mRNA in many organs for weeks. Batch-dependent heterogeneity in the toxicity of mRNA vaccines was found in Denmark. Simultaneous onset of excess mortality and COVID-19 vaccination in Germany provides a safety signal warranting further investigation. Despite these concerns, clinical trial data required to further investigate these associations are not shared with the public.
Autopsies to confirm actual death causes are seldom done. Governments may be unable to release their death data with detailed stratification by cause, although this information could help indicate whether COVID-19 infection, indirect effects of containment measures, COVID-19 vaccines or other overlooked factors play an underpinning role.
This absence of detailed cause-of-death data for certain Western nations derives from the time-consuming procedure involved, which entails assembling death certificates, coding diagnoses and adjudicating the underlying origin of death. Consequently, some nations with restricted resources assigned to this procedure may encounter delays in rendering prompt and punctual cause-of-death data. This situation existed even prior to the outbreak of the pandemic.
A critical challenge in excess mortality research is choosing an appropriate statistical method for calculating the projected baseline of expected deaths to which the observed deaths are compared. Although the analyses and estimates in general are similar, the method can vary, for instance, per length of the investigated period, nature of available data, scale of geographic area, inclusion or exclusion of past influenza outbreaks, accounting for changes in population ageing and size and modelling trend over years or not.
Our analysis of excess mortality using the linear regression model of Karlinsky and Kobak varies thus to some extent from previous attempts to estimate excess deaths. For example, Islam et al conducted an age and sex-disaggregated time series analysis of weekly mortality data in 29 high-income countries during 2020. They used a more elaborate statistical approach, an over dispersed Poisson regression model, for estimating the baseline of expected deaths on historical death data from 2016 to 2019. In contrast to the model of Karlinsky and Kobak, their baseline is weighing down prior influenza outbreaks so that every novel outbreak evolves in positive excess mortality.
Islam’s study found that age-standardised excess death rates were higher in men than in women in nearly all nations. Alicandro et al investigated sex and age-specific excess total mortality in Italy during 2020 and 2021, using an over dispersed Poisson regression model that accounts for temporal trends and seasonal variability. Historical death data from 2011 to 2019 were used for the projected baseline.
When comparing 2020 and 2021, an increased share of the total excess mortality was attributed to the working-age population in 2021.
Excess deaths were higher in men than in women during both periods. Msemburi et al provided WHO estimates of the global excess mortality for its 194 member states during 2020 and 2021. For most countries, the historical period 2015 to 2019 was used to determine the expected baseline of excess deaths. In locations missing comprehensive data, the all-cause deaths were forecasted employing an overdispersed Poisson framework that uses Bayesian inference techniques to measure incertitude. This study describes huge differences in excess mortality between the six WHO regions.
Paglino et al used a Bayesian hierarchical model trained on historical death data from 2015 to 2019 and provided spatially and temporally granular estimates of monthly excess mortality across counties in the USA during the first 2 years of the pandemic. The authors found that excess mortality decreased in large metropolitan counties but increased in non-metropolitan counties. Ruhm examined the appropriateness of reported excess death estimates in the USA by four previous studies and concluded that these investigations have likely understated the projected baseline of excess deaths and therewith over estimated excess mortality and its attribution to non COVID causes.
Ruhm explains that the overstatement of excess deaths may partially be explained by the fact that the studies did not adequately take population growth and age structure into account. Although all the above-mentioned studies used more elaborate statistical approaches for estimating baseline mortality, Karlinsky and Kobak argue that their method is a trade-off between suppleness and chasteness. It is the simplest method to captivate seasonal fluctuation and annual trends and more transparent than extensive approaches. This study has various significant limitations. Death reports may be incomplete due to delays. It may take weeks, months or years before a death is registered. Four nations still lack all-cause mortality reports for 1 to 4 months. Some nations issue complete data with profound arrears, whereas other nations publish prompt, yet incomplete data. The presented data, especially for 2022, are thus preliminary and subject to backward revisions. The more recent data are usually more incomplete and therefore can undergo upward revisions over time. This implies that several of the reported excess mortality estimates can be underestimations.
The completeness and reliability of death registration data can also differ per nation for other reasons. The recorded number of deaths may not depict all deaths accurately, as the resources, infrastructure and registration capacity may be limited in some nations. Most countries report per week, but some per month. Weekly reports generally provide the date of death, whereas monthly reports often provide the date of registration. Weekly and monthly reports may not be entirely comparable. Our data are collected at a country level and provide no detailed stratification for sociodemographic characteristics, such as age or gender. In conclusion, excess mortality has remained high in the Western World for three consecutive years, despite the implementation of COVID-19 containment measures and COVID-19 vaccines. This is unprecedented and raises serious concerns.
During the pandemic, it was emphasised by politicians and the media on a daily basis that every COVID-19 death mattered and every life deserved protection through containment measures and COVID-19 vaccines. In the aftermath of the pandemic, the same morale should apply. Every death needs to be acknowledged and accounted for, irrespective of its origin. Transparency towards potential lethal drivers is warranted. Cause-specific mortality data therefore need to be made available to allow more detailed, direct and robust analyses to determine the underlying contributors. Postmortem examinations need to be facilitated to allot the exact reason for death. Government leaders and policymakers need to thoroughly investigate underlying causes of persistent excess mortality and evaluate their health crisis policies.
Dissemination to participants and related patient and public communities.
We will disseminate findings through a press release on publication and contact government leaders and policy makers to raise awareness about the need to investigate the underlying causes of persistent excess mortality.
One hundred and Four references.
Figure 1.
Excess mortality and cumulative excess mortality in the Western World (n equals 47 countries). Preliminary and incomplete all-cause mortality reports are available for 2022.
Figure 2.
Excess mortality P-scores per country in the Western World (n equals 47 countries). Preliminary and incomplete all-cause mortality reports are available for 2022.
Figure 3 Excess mortality P-score curves of six countries in the Western World. Preliminary and incomplete all-cause mortality reports are available for 2022.
Figure 4.
Map of excess mortality P-scores in the Western World (n equals 47 countries). Preliminary and incomplete all-cause mortality reports are available for 2022.
-
 10:17
10:17
Dermatologist Dr. Dustin Portela
1 day ago $3.56 earnedOlay Cleansing Melts: Dermatologist's Honest Review
30.7K -
 1:02:20
1:02:20
Trumpet Daily
1 day ago $13.05 earnedObama’s Fake World Comes Crashing Down - Trumpet Daily | Dec. 20, 2024
16.5K18 -
 6:29
6:29
BIG NEM
18 hours agoCultivating God Mode: Ancient Taoist NoFap Practices
9.45K3 -
 30:53
30:53
Uncommon Sense In Current Times
1 day ago $0.88 earned"Pardon or Peril? How Biden’s Clemency Actions Could Backfire"
12.2K -
 40:01
40:01
CarlCrusher
16 hours agoSkinwalker Encounters in the Haunted Canyons of Magic Mesa - ep 4
22.4K2 -
 59:44
59:44
PMG
1 day ago $2.20 earned"BETRAYAL - Johnson's New Spending Bill EXPANDS COVID Plandemic Powers"
38K8 -
 6:48:50
6:48:50
Akademiks
14 hours agoKendrick Lamar and SZA disses Drake and BIG AK? HOLD UP! Diddy, Durk, JayZ update. Travis Hunter RUN
156K28 -
 11:45:14
11:45:14
Right Side Broadcasting Network
9 days agoLIVE REPLAY: TPUSA's America Fest Conference: Day Three - 12/21/24
345K28 -
 12:19
12:19
Tundra Tactical
15 hours ago $12.90 earnedDaniel Penny Beats Charges in NYC Subway Killing
66.1K12 -
 29:53
29:53
MYLUNCHBREAK CHANNEL PAGE
1 day agoUnder The Necropolis - Pt 1
153K52