Premium Only Content
MHRA has indeed become an enabler for the pharmaceutical interests
We feel compelled to conclude that the MHRA has indeed become an enabler for the pharmaceutical interests or patient safety
industry, with patient safety no longer being its primary concern.
Medicines regulator failed to flag Covid vaccine side effects,
and must be urgently investigated.
All-party parliamentary group, (APPG) on Pandemic Response and Recovery,
believe MHRA were aware of heart and clotting issues,
in February 2021,
but did not highlight the problems for several months
https://appgpandemic.org/news/mhra-letter-health-select-committee
We write regarding serious concerns about the approach of the Medicines and Healthcare Products Regulatory Agency (MHRA),
to patient safety and also problems in a system that,
far from protecting patients,
continues to put them at serious risk.
Primodos, sodium valproate and pelvic mesh
We also believe that the MHRA is at the heart of these far wider endemic failings,
and that those cited in this letter merely represent the tip of a sizeable iceberg of failure.
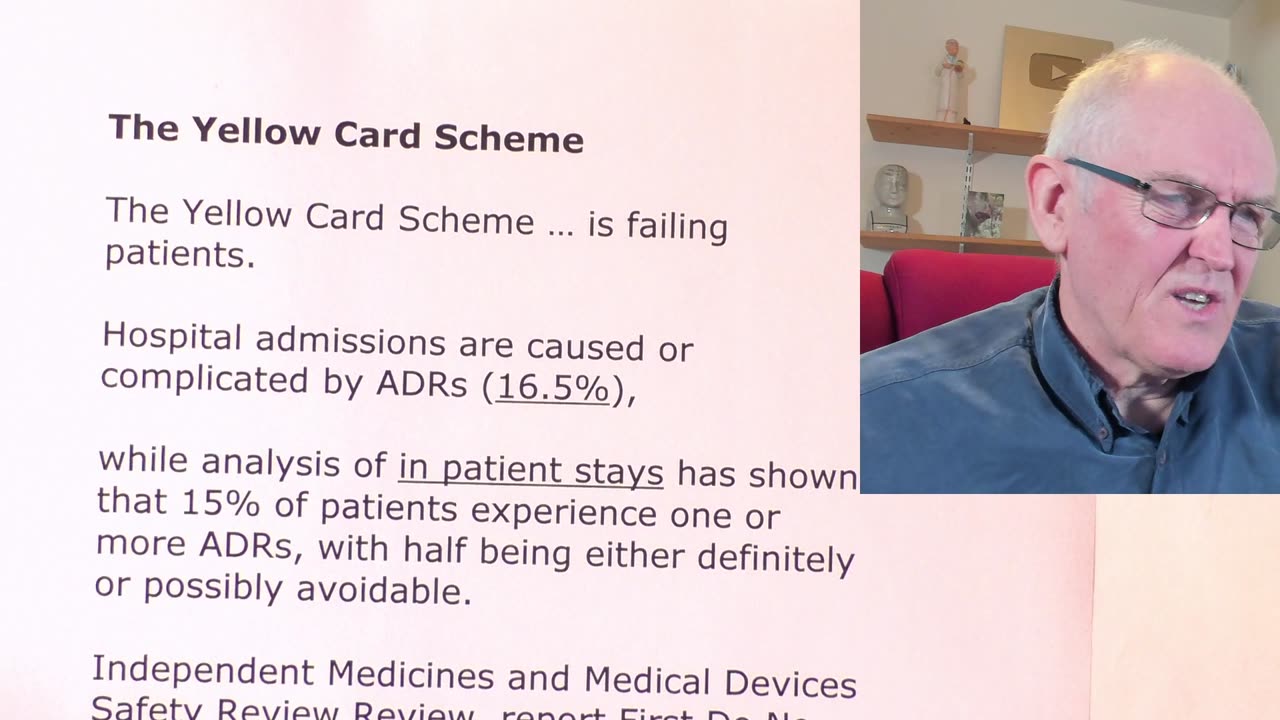
The Yellow Card Scheme
The Yellow Card Scheme … is failing patients.
Hospital admissions are caused or complicated by ADRs (16.5%),
while analysis of in patient stays has shown that 15% of patients experience one or more ADRs, with half being either definitely or possibly avoidable.
Independent Medicines and Medical Devices Safety Review Review, report First Do No Harm:
We heard about a system that cannot be relied upon to identify promptly significant adverse outcomes arising from a medication or device,
it is clear that there is gross under-reporting,
and our complaints systems are both too complex and too diffuse to allow early signal detection.
Under-reporting hinders the ability to detect signals and assign causation.
The cost to patient safety of such an unreliable system can be measured in the needless fatalities,
the considerable burden on the quality of life for survivors,
and a £2.2 billion strain on NHS England alone.
Only one in 12 patients are aware that they can report a suspected ADR.
A 2006 systemic review
https://pubmed.ncbi.nlm.nih.gov/16689555/
The rate of under-reporting of adverse events was, on average, 94% and possibly as high as 98%,
meaning possibly only two in every 100 ADRs were reported to the MHRA.
For example, a survey of UK pharmacists suggested they lack interest in, and do not promote, direct patient reporting.
Only 19% of the respondents displayed a poster promoting the Yellow Card Scheme in their pharmacy.
2023, analysis of anticoagulants
https://pubmed.ncbi.nlm.nih.gov/37269441/
Reporting of gastrointestinal bleeds
North West of England Hospital Trust recorded 12,013 bleed-related emergency admissions.
Of these, 1,058 were taking DOAC anticoagulants.
Only six DOAC Yellow Card reports (0.56% of the possible) were made by the Trust during the period.
Conflicts of Interest and Transparency
From FDA to MHRA: are drug regulators for hire?
https://www.bmj.com/content/377/bmj.o1538
The regulator-industry revolving door
Proportion of covid-19 vaccine committee members that declared financial COIs
UK, HMRA, 32%
Australia, TGA, 50%
March 2022, Dame June Raine, Chief Executive of the MHRA
agency’s transition from “the watchdog to the enabler”
does little to quell suspicions of conflicts and the implications for patient safety and cannot be overlooked.
MHRA’s responses to Freedom of Information (FOI) requests.
Between 2008 and 2017,
only 41% of requests were successful.
Since 2019, the number of requests has seen a substantial increase from 609 to 1,609 in 2021,
likely due to concerns about the regulation of Covid-19 vaccinations,
with 76% of these requests answered outside the 20 working days statutory response time.
Often exemptions were applied or vague or evasive responses were received.
The Medicines and Healthcare products Regulatory Agency
from regulatory approval to post marketing pharmacovigilance the MHRA has a history of failing patients
The MHRA does not attempt to assess or compare the safety of different vaccines
MHRA “does not hold a process for the investigation and follow up of individual Yellow Card reports”
MHRA only followed up some 54% of deaths reported in yellow cards as possibly linked to exposure to one of the Covid-19 vaccines.
Two months later, 7 May, (2021) the MHRA withdrew AZ for under 40s, but only after further needless deaths
What conclusions are we to draw about the seeming unwillingness of a regulator, largely funded by those it regulates, to disclose data to the same public it professes to protect?
We feel compelled to conclude that the MHRA has indeed become an enabler for the pharmaceutical industry, with patient safety no longer being its primary concern.
-
 14:38
14:38
Dr. John Campbell
4 days agoVaccine Juggernaut
17.1K80 -
 2:21:11
2:21:11
Nerdrotic
13 hours ago $30.22 earnedDown the Rabbit Hole with Kurt Metzger | Forbidden Frontier #090
123K22 -
 2:41:13
2:41:13
vivafrei
18 hours agoEp. 251: Bogus Social Security Payments? DOGE Lawsduit W's! Maddow Defamation! & MORE! Viva & Barnes
246K273 -
 1:19:23
1:19:23
Josh Pate's College Football Show
11 hours ago $4.58 earnedBig Ten Program Rankings | What Is College Football? | Clemson Rage| Stadiums I Haven’t Experienced
66K1 -
 LIVE
LIVE
Vigilant News Network
16 hours agoBombshell Study Reveals Where the COVID Vaccine Deaths Are Hiding | Media Blackout
2,195 watching -
 1:17:59
1:17:59
Sarah Westall
12 hours agoDOGE: Crime & Hysteria bringing the Critics & the Fearful - Plus new CDC/Ukraine Crime w/ Dr Fleming
74.6K7 -
 45:39
45:39
Survive History
18 hours ago $10.41 earnedCould You Survive in the Shield Wall at the Battle of Hastings?
75.3K6 -
 1:50:28
1:50:28
TheDozenPodcast
16 hours agoViolence, Abuse, Jail, Reform: Michael Maisey
110K4 -
 23:01
23:01
Mrgunsngear
1 day ago $6.55 earnedWolfpack Armory AW15 MK5 AR-15 Review 🇺🇸
93.8K12 -
 25:59
25:59
TampaAerialMedia
1 day ago $4.34 earnedUpdate ANNA MARIA ISLAND 2025
60K4